Operational efficiency in healthcare is more than a buzzy catchphrase. It is the backbone of hospitals and patient care quality at large, and failing to invest in it has significant repercussions both from a business and a patient care perspective.
Underutilizing medical equipment can cost upwards of $12,000 a year per bed. Unoptimized systems result in monetary losses, strained resources, reduced staff morale, and, most importantly, jeopardized patient health and safety.
To prevent this, your organization must discover current inefficiencies and work to reduce them. This will allow you to maximize resources, understand existing barriers, improve operations, and provide the best possible patient outcomes.
Operational Efficiency in Healthcare: Practical Examples
By streamlining operations and technology, healthcare delivery organizations (HDOs) can improve patient conditions, meet operations and business outcomes, and drive overall patient care.
Consider monitoring machines, which assist medical professionals in tracking patient health and respond promptly to any changes. Managing these machines can be cumbersome and time-consuming because there is a lot of essential data to monitor and analyze. Operational efficiency enhancements streamline monitoring machines' management by automating data processing and integration, reducing manual oversight, and minimizing technical issues.
Patient communication is another critical area for operational improvements. Tools like automated appointment reminders, patient portals, and real-time response systems can improve interactions, leaving medical professionals free to focus on providing high-quality care.
Finally, operational efficiency is crucial to maintaining regulatory compliance, both in staying compliant and showing proof of compliance to auditors and local regulatory bodies. Tracking, tracing, and documenting the status of medical devices, clinical assets, and facilities is critical to maintaining compliance with regulations such as HHS 405(d).
Source: https://learn.g2.com/healthcare-operations
Barriers to Operational Efficiency in Healthcare
1. Outdated Technology Infrastructure
Healthcare organizations depend on a wide range of technology tools for operations. From software to manage patient information to clinical devices to facilitate patient care, managing many devices and systems requires significant time and money.
Over 90% of healthcare executives say technology consolidation is essential to improving operational efficiency. Yet, 80% are still in the planning or initial stages of consolidation.
An abundance of software tools or assets constantly requiring service or replacement, combined with a myriad of infrequently used medical devices, can lead to significant losses in time and energy. Pair this with the fact that many devices are outdated, legacy equipment, and you realize the vast challenges to consolidation.
2. Cybersecurity Threats
Cyber attacks like malware, ransom, or even clone phishing attacks can significantly derail operational efficiency. Healthcare organizations manage vast volumes of sensitive information that, if compromised, can jeopardize patient trust and operational integrity.
With cyber-attacks becoming increasingly frequent and sophisticated, healthcare organizations must invest in advanced cyber-physical systems (CPS) protection platforms and medical device risk management to secure devices connected to the network.
Source: https://online.maryville.edu/blog/healthcare-cybersecurity/
3. Regulatory compliance
Another hurdle facing healthcare organizations is complying with the ever-changing landscape of regulations meant to safeguard patient safety. Without a system to comply with in-patient care standards, device management practices, and cybersecurity regulations, you risk failing to meet regulatory standards and exposing your organization to severe operational efficiency risks.
4. Inefficient workflow processes
The complexity of healthcare operations often leads to a lack of standardized processes, causing delays and redundancies that can risk patient care outcomes. Additionally, inefficient workflows can increase healthcare costs and workload for healthcare professionals.
5. Resource management challenges
Misallocating and underutilizing critical assets can significantly hinder operational efficiency. For instance, improper medical equipment management can result in delays due to equipment shortages or excessive maintenance costs, further disrupting workflows and increasing operational strain. Another challenge that hospitals and healthcare organizations face is the lack of cybersecurity talent within their IT resources due to staffing constraints, which is detrimental to managing attack surfaces.
7 Essential Tips for Improving Operational Efficiency
1. Dynamically Manage Device Inventory and Utilization
A comprehensive inventory is critical to improving asset visibility and understanding how your assets connect within the network. For greater visibility, choose a solution that integrates with your asset management solutions, such as CMMS/CMDB.
Within your asset inventory, you can monitor device utilization to understand better which assets are approaching end-of-life, which could lead to more significant cybersecurity risks. This data could also inform you of device distribution and hours, utilization rate, and average number of examinations. Biomed teams, in particular, can track and view utilization reports based on the type of medical device, cutting down on time and improving basic efficiencies.
2. Track and Optimize Device Locations
Knowing exactly where your devices are at all times is vital. The ability to seamlessly track the location of devices across multiple sites will allow your team to keep better tabs on mobile equipment or lost devices. Integrating location services with existing tools can even eliminate the need for costly location tracking solutions such as real-time locating systems (RTLS).
3. Enhance Device Procurement and Operations
Measure and assess the risk postures of device types in your fleet to make better-informed purchasing decisions. Utilize industry benchmarks and usage data to right-size your device fleet, ensuring you have the appropriate quantity and types of devices needed for your specific healthcare environment.
Device procurement data can help you balance device distribution across various departments or locations and renegotiate lease and maintenance agreements for better terms. By aligning procurement strategies with actual usage patterns and industry standards, you can enhance cost efficiency and improve device reliability.
4. Assess and Maintain Device Usage and Lifecycles
Understanding device usage and life cycles through asset management is critical to ensuring patient safety. Knowing that a device will work correctly whenever needed is essential to preserving an environment of care. Access device lifecycles, determine end-of-life or unsupported operating systems, and identify or resolve high-risk devices that can still perform their clinical function.
5. Optimize Capital Planning
Finances may not spring to mind immediately when considering operational efficiency, but understanding how the usage of devices can be tied directly to improving ROI and capital planning for your organization.
Analyzing detailed reports on device utilization and lifecycle status can help you make informed decisions about necessary device replacements and upgrades. You can also notify your finance team about necessary expenses early on, ensuring adequate funds are allocated for critical investments. Effective capital planning allows your healthcare organization to optimize resource allocation and achieve the most significant impact on operational efficiency.
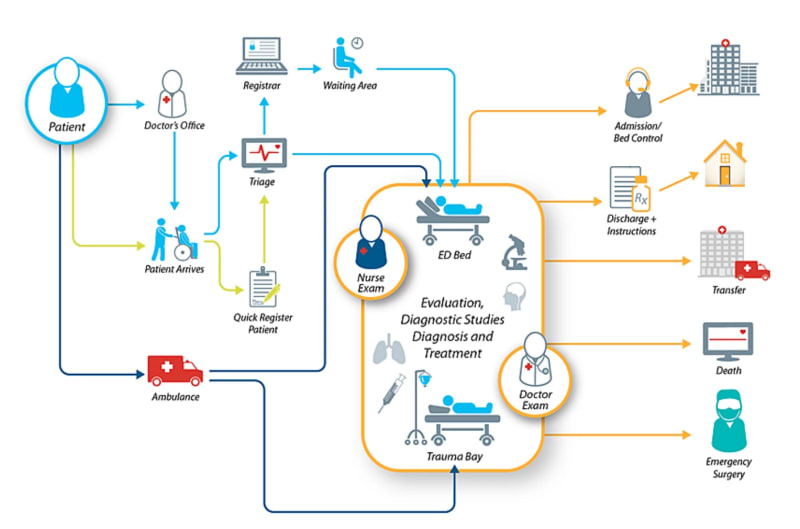
6. Improve Patient Flow Management
Patient flow management is about managing the movement of patients, devices, and materials through the healthcare facility from the moment they walk through the door until they leave. It is critical to have the right tools to balance this flow.
Source: https://centrak.com/resources/blog/optimized-patient-flow-in-the-emergency-department
7. Improve Device Operations and ROI
Efforts to save time and streamline tasks are always warranted in improving ROI and maintaining the right level of operational efficiency in healthcare. Automate time-intensive tasks via CMMS reconciliation and auditing so biomed teams can focus on higher-value objectives. You can achieve this by leveraging operational efficiency recommendations explicitly automated in the platform to quickly and efficiently derive ROI.
Implement Operational Efficiency Strategies with Claroty xDome
When done correctly, improved operational efficiency can lead to better patient outcomes, better maintenance of medical devices and assets, enhanced financial planning, and overall better morale in your organization.
The key to enabling most of these essential strategies starts with the right platform to monitor and manage your devices - a comprehensive platform - like Claroty xDome. From robust cybersecurity protection for medical devices and building automation systems (BAS) to critical information about device usage and lifecycles, Claroty xDome offers all the information you need to start making better operational decisions.
To learn more about Claroty xDome's functionalities, schedule a demo with a team member and get started improving your healthcare organization's operational efficiency.






Top comments (0)